Coronary Angioplasty and Stenting
Understanding Coronary Angioplasty and Stenting:
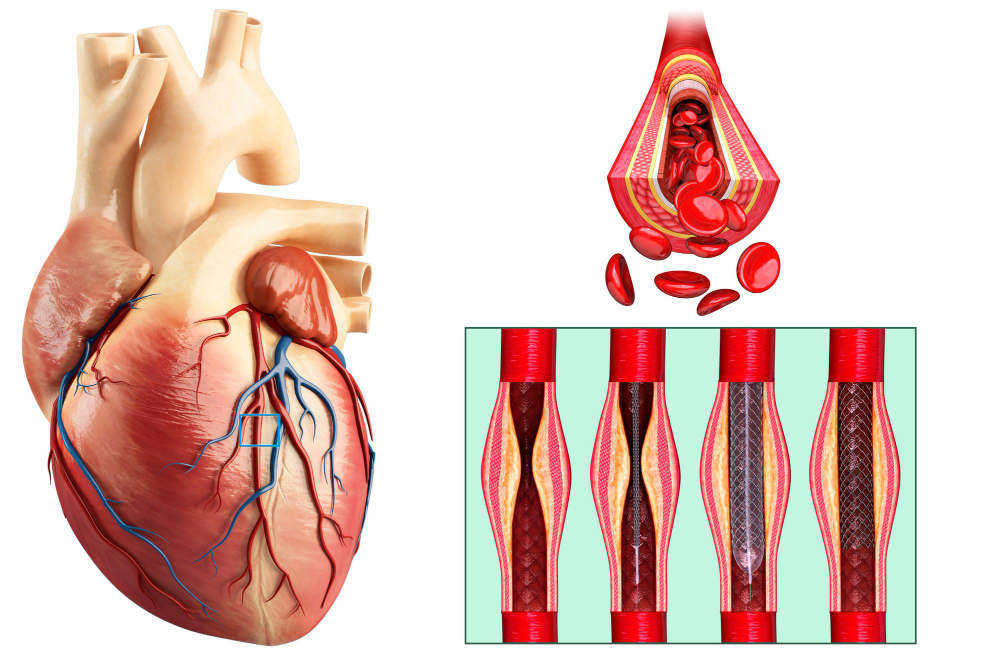
Coronary angioplasty and stenting is a minimally invasive procedure used to treat coronary artery disease (CAD), which involves the narrowing or blockage of the coronary arteries that supply oxygen-rich blood to the heart muscle. During the procedure, a thin, flexible tube called a catheter is inserted into a blood vessel, typically in the groin or wrist, and guided to the site of the blockage in the coronary artery. Once in place, a small balloon at the tip of the catheter is inflated to compress the plaque and widen the narrowed artery, restoring blood flow. Additionally, a stent—a mesh-like metal tube—is inserted to hold the artery open and prevent it from narrowing again.
Procedure:
- Preparation: Before the procedure, patients may undergo imaging tests such as coronary angiography to assess the severity and location of the blockage in the coronary arteries.
- Anesthesia: Coronary angioplasty and stenting are usually performed under local anesthesia, with sedation to help the patient relax and remain comfortable during the procedure.
- Insertion of Catheter: A catheter is inserted into a blood vessel, typically in the groin or wrist, and threaded through the arteries to reach the site of the coronary artery blockage.
- Angioplasty: Once the catheter reaches the blockage, a small balloon at the tip of the catheter is inflated to compress the plaque and widen the narrowed artery, restoring blood flow.
- Stent Placement: After angioplasty, a stent is deployed to hold the artery open and prevent it from narrowing again. The stent remains permanently in place to maintain adequate blood flow to the heart muscle.
- Closure of Incision: Once the procedure is complete, the catheter is removed, and the incision site is closed with sutures or a closure device. Pressure may be applied to the site to prevent bleeding.
Aftercare Following Coronary Angioplasty and Stenting: After undergoing coronary angioplasty and stenting, patients typically require a period of recovery and follow-up care. Here are some key aspects of aftercare:
Hospital Stay: The length of hospital stay may vary depending on individual patient factors and the presence of any complications during or after the procedure. In many cases, patients can expect to stay in the hospital for observation overnight.
Activity Restrictions: Patients may be advised to avoid strenuous activities and heavy lifting for a period of time following the procedure to allow for proper healing. Light activities and gradual return to normal daily routines are usually encouraged.
Medications: Patients may be prescribed medications such as antiplatelet agents (e.g., aspirin, clopidogrel) to prevent blood clots and reduce the risk of complications following coronary angioplasty and stenting. Compliance with medication regimens and regular follow-up appointments with healthcare providers are important for optimal recovery.
Lifestyle Modifications: Adopting heart-healthy lifestyle habits such as maintaining a balanced diet, engaging in regular physical activity, quitting smoking, limiting alcohol intake, and managing stress can help improve overall cardiovascular health and reduce the risk of future coronary artery disease.
Follow-up Visits: Scheduled follow-up visits with a cardiologist or cardiac surgeon are essential to monitor healing, assess coronary artery function, and address any concerns or complications that may arise. These visits may include imaging tests such as coronary angiography or cardiac stress testing to evaluate the effectiveness of the procedure and detect any signs of restenosis (re-narrowing) of the coronary artery.
