Valvular Heart Disease
Understanding Valvular Heart Disease:
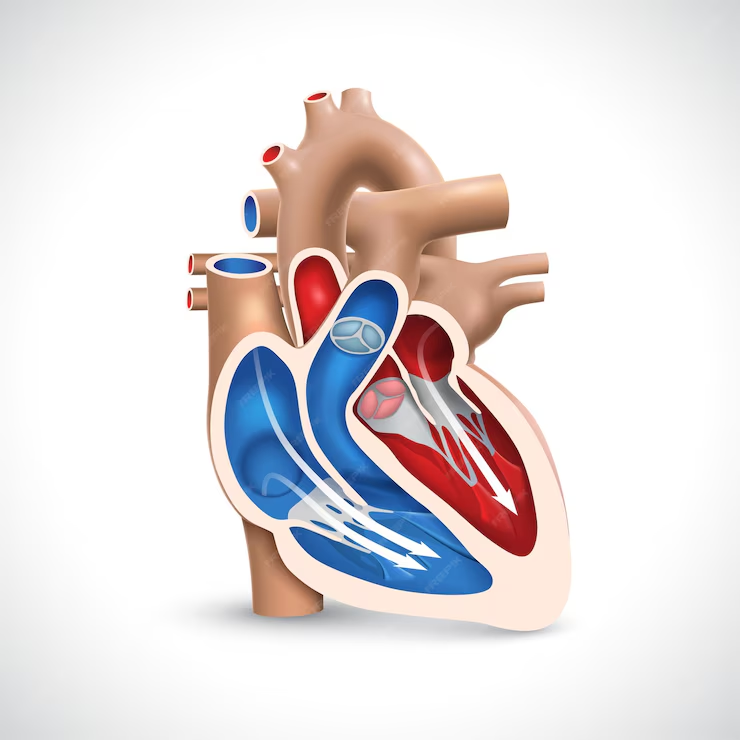
Valvular heart disease refers to conditions that affect one or more of the heart’s valves, impairing their function and disrupting blood flow within the heart. The heart valves, including the mitral valve, aortic valve, tricuspid valve, and pulmonary valve, play a crucial role in regulating blood flow between the heart’s chambers and throughout the body. Valvular heart disease can manifest as valve stenosis (narrowing), valve regurgitation (leakage), or a combination of both, leading to symptoms such as shortness of breath, chest pain, fatigue, palpitations, and fluid retention.
Diagnosis: Diagnosing valvular heart disease typically involves a combination of medical history review, physical examination, and diagnostic tests such as:
- Echocardiography (echo)
- Electrocardiography (ECG/EKG)
- Cardiac MRI
- Cardiac CT scan
- Transesophageal echocardiography (TEE)
- Cardiac catheterization
These tests help evaluate the structure and function of the heart valves, assess the severity of valve dysfunction, and identify underlying causes or contributing factors such as congenital abnormalities, degenerative changes, infective endocarditis, or rheumatic fever.
Management Strategies: Managing valvular heart disease focuses on relieving symptoms, preventing complications, and optimizing heart function. Here are key components of valvular heart disease management:
Medication Management:
- Medications such as diuretics, ACE inhibitors, beta-blockers, and anticoagulants may be prescribed to manage symptoms, control blood pressure, prevent blood clots, and reduce the risk of complications such as heart failure or stroke.
Valve Repair or Replacement:
- Depending on the severity and type of valve dysfunction, surgical interventions such as valve repair or replacement may be necessary. Valve repair aims to restore the valve’s function using surgical techniques such as annuloplasty, leaflet repair, or commissurotomy. Valve replacement involves replacing the damaged valve with a mechanical valve, tissue valve (bioprosthesis), or transcatheter valve (TAVR).
Transcatheter Interventions:
- For select patients deemed high-risk for traditional open-heart surgery, minimally invasive transcatheter interventions such as transcatheter aortic valve replacement (TAVR) or transcatheter mitral valve repair (TMVR) may be considered. These procedures involve inserting a catheter through a small incision and deploying a prosthetic valve or repair device to improve valve function.
Lifestyle Modifications:
- Adopting heart-healthy lifestyle habits such as maintaining a balanced diet, engaging in regular physical activity, quitting smoking, limiting alcohol intake, and managing stress can help improve overall cardiovascular health and reduce the risk of complications associated with valvular heart disease.
Regular Monitoring and Follow-up:
- Regular follow-up visits with a healthcare provider are essential to monitor symptoms, assess valve function, and adjust management strategies as needed.
